Denied Medical Claims: Top Reasons, Codes & Fixes | Complete Guide
By Billmate
June 24, 2025, 6:10 a.m.
Learn how to fix denied medical claims with our guide to common denial codes like CO-16, CO-4, and CO-15. Discover prevention tips & appeal strategies to maximize revenue.
What Are Denied Claims in Medical Billing?
A denied claim in medical billing occurs when a payer processes your claim but refuses payment. Unlike rejected claims (which fail submission due to errors), denied claims enter the adjudication system but get declined for reasons like:
-
Missing information
-
Policy violations
-
Coding mistakes
-
Unmet requirements
Example: Your clinic submits a claim, only to receive a CO‑16 incomplete information denial weeks later - perhaps due to a missing modifier or incorrect patient details.
Why Understanding Denied Claims Is Crucial
Denied claims create cash flow problems, especially for small practices. Consider these facts:
-
Up to 65% of denied claims are never resubmitted
-
Each denial increases administrative costs
-
They delay your revenue cycle
Understanding denial codes medical billing helps you:
-
Improve claim acceptance rates
-
Reduce rework
-
Ensure timely payments
-
Enhance patient financial experiences
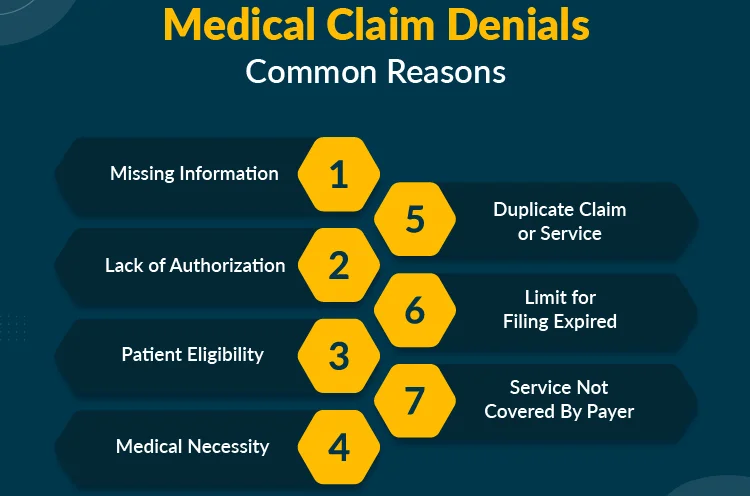
Common Claim Denial Reasons
1. Missing Information (CO‑16 Denial)
The Problem: Blank fields or incorrect data (e.g., missing DOS or wrong insurance ID)
Solution:
-
Use automated claim scrubbers
-
Train staff on documentation requirements
2. Duplicate Claims (CO‑18 Denial)
The Problem: Submitting the same claim multiple times
Fix:
-
Configure billing software with duplicate alerts
3. Expired Coverage (CO‑27 Denial)
The Problem: Services rendered after policy expiration
Prevention:
-
Verify insurance at every visit
4. Late Submission (CO-29 Denial)
The Problem: Missing payer filing deadlines (typically 90-180 days)
Avoidance:
-
Submit claims weekly
-
Use timely filing alerts
Top Medical Billing Denial Codes Explained
CO‑4: Missing Modifier Claim Denial
Occurs when required modifiers are omitted
Tip: Review CPT guidelines for modifier requirements
CO‑11: Coding Error Denial
Results from procedure-diagnosis code mismatches
Solution: Conduct regular coding audits
CO‑15: Prior Authorization Denial
Happens when services lack required authorizations
Fix: Implement prior auth tracking systems
CO-22: Coordination of Benefits Denial
Occurs when billing the wrong primary insurer
Best Practice: Verify COB for every patient
Medical Necessity Denials
Definition: When payers deem services unnecessary
Appeal Strategy:
-
Submit supporting medical records
-
Highlight failed prior treatments
-
Use appropriate ICD-10 codes
How to Fix Denied Medical Claims
-
Identify the denial code from EOB/ERA
-
Analyze original claim for errors
-
Collect supporting documents
-
Resubmit with corrections
-
Track resubmission status
-
File appeal if necessary
Denial Management Best Practices
1. Maintain Accurate Patient Data
-
Verify demographics
-
Confirm insurance details
2. Conduct Real-Time Eligibility Checks
Prevent CO‑27 and CO‑22 denials
3. Code Precisely
Avoid CO‑11 and CO‑4 errors through:
-
Regular coding audits
-
Staff training
4. Track Authorizations
Use software reminders for services requiring prior authorization
Technology to Reduce Denials
-
Claim scrubbing software
-
EHR-PMS integration
-
Real-time eligibility tools
-
Analytics dashboards
Conclusion
Understanding denial codes medical billing and implementing preventive measures can significantly reduce claim denials. Focus on:
-
Accurate documentation
-
Timely submissions
-
Proper coding
-
Effective appeals
FAQs
Q: What's the most common reason for claim denials?
A: CO‑16 incomplete information denial
Q: How to avoid CO‑4 denials?
A: Always verify required modifiers
Q: Why is prior authorization important?
A: Prevents CO‑15 prior authorization denials
Q: How often should I review denials?
A: Weekly for patterns, monthly for deep audits
What to read next

By Billmate | July 19, 2025
Mastering Medical Billing in 2025: Trends, Tools, and Tactics for Success
Explore the top medical billing trends in 2025 including CPT code changes, HIPAA-compliant software…

By Billmate | July 18, 2025
Your 2025 Guide to Medical Billing and Coding: Jobs, Salaries & Online Courses with Billmate
Discover everything you need to know about medical billing and coding in 2025—career paths, salarie…

By Billmate | July 17, 2025
Ultimate Guide to Telemedicine Billing in the USA
Learn how to optimize telemedicine billing and medical coding in the USA with Billmate. Maximize re…
Join our team to be a part
of our story
Learn more about our career, education and
posting jobs, and
submit simple application.

